Evaluation and comparison of postoperative levels of serum bilirubin, serum transaminases and alkaline phosphatase in laparoscopic cholecystectomy versus open cholecystectomy
Introduction
Biliary calculosis is one of the most frequent diseases and surgical interventions are commonly performed on bile ducts. These patients should either undergo open cholecystectomy (OC) or the procedure performed with a gasless or low pressure laparoscopic technique. Patients with cirrhosis and portal hypertension are at risk for two reasons: low peripheral resistance and the risk of bleeding that is difficult to control during the procedure. Cholecystectomy in these patients should not be attempted laparoscopically. The adverse physical effects of intra abdominal hypertension were reviewed in detail recently (1). Another study correlated intra-abdominal pressure in patients undergoing laparoscopic cholecystectomy (LC) with blood flow to the liver was measured using a laser-Doppler technique, and tonometrically assessed gastric perforation. Both hepatic and gastric microcirculation fell significantly during LC performed with a pneumoperitoneum of 12 mmHg, indicating splanchnic ischemia (2). Recently few studies have shown rise in parameters of liver function test (LFT) following LC and have implicating hepatic hypoperfusion and ischemia. It has been noticed that following LC, the serum level of certain liver enzymes rise markedly in patients which were preoperatively normal (3-5).
The changes in LFTs after LC (total 55 patients) were compared with those after OC (total patients 16). During the LC, the intraabdominal pressure was maintained at 14-15 mmHg. Alanine transaminase (ALT) doubled in 58.2% of the patients undergoing LC while it doubled in only 6.3% of the patients of OC group (P=0.00027) after 48 hours. Aspartate transaminase (AST) doubled in 38.2% of the patients in the LC group versus only 6.3% in the OC group (P=0.01579). The value of total bilirubin (TBIL), alkaline phosphatase (ALP), Serum Albumin was not altered in any group (6). Once considered as incidental elevation of liver enzymes such as AST and ALT after non complicated LC has become a well-known finding (7,8). Carbon dioxide (CO2) has high hematic solubility and can cause hypercapnia and respiratory acidosis. Additionally an intra-abdominal pressure of 12-14 mmHg of CO2 was higher than the normal portal blood pressure of 7-10 mmHg and was therefore capable of reducing portal blood flow and causing alteration in hepatic function (9,10).
It seems the free radicals are generated at the end of laparoscopic procedures, possibly as result of an ischaemia reperfusion phenomenon induced by inflation and deflation of pneumoperitoneum. Free radicals can damage tissue and organs especially the kupffer and endothelial cells of the hepatic sinusoids (11,12). Because hepatic hypoperfusion induced by laparoscopy has been underestimated, the aim of this study is to review the numerous factors influencing hepatosplanchnic blood flow during laparoscopy and to alert clinicians to the adverse consequences of hepatic hypoperfusion in high risk patients undergoing this procedure (13,14). Unisa et al. studied that prevalence of gallstones was 4.15% in rural Gangetic basin; more in females 5.59% than males 1.99% (P<0.05) (15). The present study has been undertaken to know the changes in LFTs after LC/OC, the incidences of such change, there relation to age, sex, duration of surgery and to know the clinical significances of such disturbances.
Materials and methods
The present study was conducted in the Department of Surgery at MMIMSR, Mullana, Ambala. A total 200 patients of cholelithiasis were included in this study from May 2012 to May 2014 by using sealed envelope technique. These cases were randomly divided into two groups (A and B) consisting of 100 cases in each group. LC was performed in group A patients and OC was performed in group B patients. Patients from 20 to 75 years of age were included in this study. Those cases diagnosed as pregnancy, common bile duct (CBD) stones, high levels of enzymes before operation, positive serology for hepatitis B or C virus were excluded. On admission, a detailed history of each patient was taken and a thorough general and local physical examination was done. The routine investigations were baseline LFTs, including ultrasonography (USG), computed tomography and wherever required MRCP was also done to rule out CBD stones. Cholecystectomy was performed under general anesthesia with intravenous anesthesia induction followed by continuous volatile anesthesia under mechanical ventilation. The study was approved by the institutional ethics committee.
Operative techniques
LC performed in group A, 12-14 mmHg of pneumoperitoneum was created and maintained by intra peritoneal CO2 insufflation with an automatic insufflator. Patient head was elevated and right side of the patient tilted towards the left side. Four ports were made; two 10 mm port-infraumbilical site, epigastrium region and two 5 mm port; right lateral, another in subcoastel region two fingers below midlaviculer area. Pneumoperitoneum was created. Calot’s triangle identified and clip was applied to the cystic duct and cystic artery by taken care not to injure the CBD. Gall bladder was removed from the liver bed with the help of diathermy.
OC was performed in Group B as routine procedure. A sand bag was kept under the right renal lumber area to raise the hypochondrium region for the purpose of easy dissection. A right subcoastel incision made and abdomen opened in layers. Gall bladder recognized cystic duct and artery ligated separately. Gall bladder was removed from the liver bed with the help of the diathermy. If any bleeding was suspected from the liver bed then gell foam was used. Drain was kept in all cases and removed when it was less than 20 mL. Third generation antibiotic ceftriaxone + sulbactum and amikacin, metrogyl were used for 2 days and if bile leakage was present then antibiotic were used for 5 days. Analgesic were given in the form of injection voveran and if required tramadol also to all the patients for two days and then put on anti-inflammatory drugs for 10 days.
Post-operative
No other medication was administered to the patients prior or after the operation except for intravenous antibiotics and pain killer for post-operative pain control. Blood samples were taken from the superficial vein before the operation as a part of routine pre-operative preparation and 24 hours after the operation for comparison of the enzyme level alterations. 3rd blood sample was taken after 72 hours. Biochemical analyses for enzymes were done using the same analyzer. The accepted normal values are; for AST, 5-40 U/L (by IFCC kinetic method), for ALT, 5-35 U/L (by IFCC kinetic method), for serum bilirubin, 0.2-1 mg/dL (Jendrassik and Grof method), for ALP, 28-112 U/L (by IFCC kinetic method using P-nitrophenylphosphate).
Enzyme levels were calculated as mean ± standard deviation (SD) for both groups and for both preoperative and post operative values. Statistical analysis included chi-square test, paired t-test, ANOVA test was done. All the observations were recorded, procedure was explained to the patient and separate consent was taken.
Observations and analysis
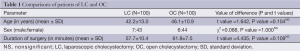
In both groups, the changes occurred in liver enzymes pre- and post-operative were noted. The mean age of the patients in the LC and OC was 42.2 and 46.1 years respectively (Table 1). The mean gender preponderance of the male: female ratio in the LC and OC was 7:43 and 6:44 respectively. Both the groups are comparable in age, sex and duration of surgery as the difference were not significant i.e., P>0.05. The most common clinical symptom was dyspepsia which was seen in all the cases of LC and in 82% of cases in OC. Pain right hypochondrium was present in 86% of cases in both LC and OC. Nausea and vomiting were observed in 78% of the cases in LC and 74% cases in OC.
Full table
Duration of surgery
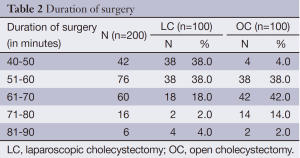
In LC the duration of surgery was taken from the time of insertion of veress needle to the time of applying last stitch while in OC group it was taken from the time of skin incision to completion of skin suturing. The mean duration of surgery in LC group was 57.7 minutes and in OC group the mean duration of surgery was 61.8 minutes, as the difference were not significant i.e., P>0.05 in both the groups (Table 2).
Full table
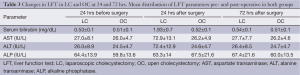
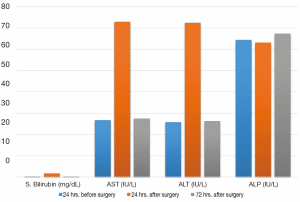
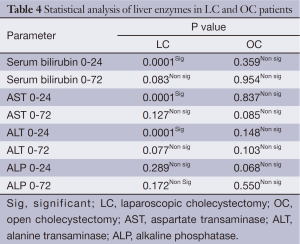
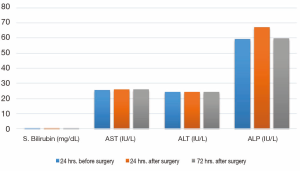
There were rise in the mean value of serum bilirubin AST and ALT after 24 hrs of surgery from the preoperative value and then again fall (near to normal value) after 72 hrs of surgery except in the mean value of ALP, which showed slight fall after 24 hrs of surgery and then slight rise after 72 hrs of surgery which was within the normal limit (Table 3, Figure 1). The study showed rise in serum bilirubin from preoperative (0 hrs) value to postoperative value (24 hrs) was significant (P=0.0001) and there was no significant rise after 72 hrs of operation. Similarly, AST and ALT showed significant rise after 24 hrs of surgery (P=0.0001) and non significant rise after 72 hrs of operation whereas ALP showed no significant rise in both after 24 and 72 hrs of surgery (Table 4). In OC group there were slight variations in the mean value of all the liver enzymes (which were within the normal range) but there were no significant rise in the mean value of them after 24 hrs of surgery (Figure 2).
Full table
Full table
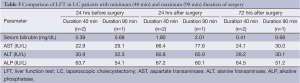
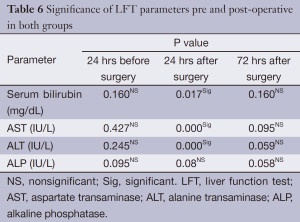
The present study showed no significant difference in serum bilirubin, AST, ALT and ALP after 24 and 72 hrs of surgery from preoperative value as the P>0.05 in all the cases. We observed that the patient undergoing LC with minimum duration of surgery (40 min) has less variation in LFT (serum bilirubin, AST, ALT) as compared to the patient undergoing LC with maximum duration of surgery (90 min) (Table 5). In our study, doubling of serum bilirubin, AST and ALT levels were seen in 22 (44%) patients, 8 (16%) patients and 10 (20%) patients respectively whereas 21 (42%) patients, 35 (70%) and 33 (66%) patients respectively showed rise of 50-100% after 24 hrs of surgery. A total of 0-50% rise seen in 7 (14%) patients for serum bilirubin, AST and ALT after 24 hrs of surgery (Table 6).
Full table
Full table
The overall rise in LFT parameters in OC group was quite low as compared to the LC group. The P value was significant when comparison was made between the mean values of LFT parameters after 24 hrs of surgery in LC and OC group except in ALP.
Discussion
Cholelithiasis and its complications are the leading cause of surgical entry into the peritoneal cavity. So widespread is this disease that it will not be out of place to say that cholecystectomy is one of the commonly performed surgical procedure. A standard-pressure of 12-14 mmHg is used in LC to create the pneumoperitoneum, which may result in variety of abnormal physiological changes involving the respiratory, cardiovascular, and hepatorenal systems. The introduction of the pneumoperitoneum causes major decreased blood flow lead to adverse glomerular filtration and tubular functions which produce abnormal biochemical parameters (2,16). By keeping the low range of pressure 8-10 mmHg for pneumoperitoneum has been shown to decrease the adverse physiological changes without affecting the outcome of surgery as in present study, pressure was kept 12-14 mmHg (2). Tan et al. (17) found statistically significant increased levels of hepatic transaminases during the first 48 hours post operation in patients undergoing LC and laparoscopic colonic resection compared to patients having open procedures. The degree of change in ALT following the operations was greater in LC patients than that in OC patients (P<0.05, D1; P<0.01, D2), so was the change between LCR and OCR patients (P<0.05, D1,7; P<0.01, D2). The change of AST due to the operations was also greater in LC patients than that in OC patients (P<0.05, D1; P<0.01, D2), and so was the change between LCR and OCR (P<0.05, D1,7; P<0.01, D2). They concluded that laparoscopic surgery may not be optimal for patients with pre-existing liver impairment. CO2 pneumoperitoneum is the most common cause for transient elevation of hepatic transaminases after laparoscopic surgery. However, if preoperative liver function was very poor, laparoscopic surgery may not be the best choice for the treatment of the patients with certain abdominal diseases (17). Omari and Bani-Hani (18) investigated the serum levels of eight parameters of liver function both before and 24 hrs after surgery in 142 consecutive patients who underwent LC, 23 patients who underwent OC and in 25 patients who underwent a conventional hernia repair. The intra abdominal pressure was maintained at 12 mmHg of carbon dioxide. It appears that the pneumoperitoneum plays a major role in these changes. The safety of the procedure must nonetheless be assessed in those with underlying liver diseases. They found that 83% of the patients showed more than 100% increase in atleast one parameter, 43% showed an increase in 2 or more parameters and 23% showed an increased in 3 or more parameters.
Another prospective study was done to investigate the effect of abdominal perfusion pressure on LFTs after LC with intra abdominal pressure of 12 mmHg. They reported that 37.5% showed more than 100% increase in atleast one parameter of liver function. Author stated that subclinical hepatic dysfunction after LC could mostly be attributed to the negative effects of pneumoperitoneum on hepatic blood flow (19). Ahmad calculated the net change between the means of the preoperative and postoperative values of LFTs by keeping the CO2 pressure was 12-15 mmHg. They noted the mean value for postoperative ALP was less than the preoperative value, which suggests very little or no change in the postoperative value of this enzyme. This finding was commonly observed in patients with preoperatively elevated LFTs. A statistically significant difference was observed between the two values Wilcoxon Signed-rank test. It is evident that the level of alteration is different for each enzyme and that most of the cases fall into the group that shows up to a 50% increase in the LFTs. This change can be labelled as mild elevation and is considered negligible by many. Increased bilirubin levels were seen in a fraction of patients; ALP was not found to increase to such a high level in study. Mild to moderate elevation in LFTs may not be associated with any deleterious effect and in the absence of clinical indications, routine postoperative or preoperative LFT is unnecessary (20).
Marakis et al. (21) reported the mean duration of surgery in LC was 55 min (range, 40-70 min). In our design, the mean duration of surgery in LC group was 57.7 minutes and in OC group the mean duration of surgery was 61.8 minutes which is non-significant (P=0.109) and made both the groups comparable. In LC group we found that the patient with minimum duration of surgery (40 min) had less elevation in liver enzymes (serum bilirubin, AST and ALT) as compared to the patient with maximum duration (90 min) of surgery.
In our study, we also adopted a strict exclusion criteria aimed at eliminating known causes of liver function disturbances (CBD pathology and chronic liver diseases) by subjecting the patients to preoperative ultrasound, by checking for hepatitis B antigen and hepatitis C antigen, preoperative LFT 24 hours before operation and prothrombin time so that any disturbances in liver function can be confidently attributed to the laparoscopic procedure itself. In present study the rise in AST and ALT were seen in >90% of the LC patients and the doubling in AST and ALT were seen in 8 patients (16%) and 10 (20%) patients respectively whereas 35 (70%) and 33 (66%) patients respectively showed rise of 50-100% after 24 hrs of surgery. 0-50% rise is seen in 7 (14%) patients for AST and ALT after 24 hrs of surgery. The rise in mean values of enzymes in our study was similar to the studies of Guven et al. (22) and Sakorafas et al. (23) (Table 7). In our study, the mean value of ALP showed slight fall after 24 hrs of surgery and then slight rise after 72 hrs of surgery which was within the normal limit. In present study, >90% patients showed rise in TBIL and doubling (i.e., >100%) in serum bilirubin levels is observed in 22 (44%) patients whereas A total of 50-100% rise is seen in 21 (42%) patients after 24 hrs of surgery. A total of 0-50% rise in TBIL is seen in 7 (14%) patients after 24 hrs of surgery from preoperative value.

Full table
Marakis et al. found that the rise in serum bilirubin in LC group was 48.4%, the preoperative mean value was 0.64±0.24 mg/dL which showed significant rise to 0.95±0.58 mg/dL 24 hours after surgery and in our study the preoperative mean value was 0.53±0.1 mg/dL which also showed significant rise to 1.93±0.7 mg/dL after 24 hours of surgery (21). Bhoorasingh et al. observed that the instillation of CO2 leads to hypercapnia which increases minute ventilation by as much as 60% and activates the sympathetic nervous system. Pneumoperitoneum raises intra-abdominal pressure which can have significant cardiovascular, respiratory and neurological effects. Changes in pulmonary function include reduction in lung volumes, increase in peak airway pressure, and decrease in pulmonary compliance secondary to increased intra-abdominal pressure and patient positioning. Moderate to severe shoulder tip pain thought to be related to stretching of the sub-diaphragmatic peritoneum after pneumoperitoneum has been reported to occur in as many as one-third of patients. Prolonged procedures may lead to hypothermia which may be offset by the use of heated or humidified gas (24).
Mohamed et al. in his study observed elevation in the levels of serum ALT and AST within 24-48 hours following operations in LMUDT (laparoscopic maneuver for undescended testicle) patients compared with those in OMUDT (open maneuver for undescended testis) patients. The degree of change in ALT following LMUDT was greater than OMUDT and this difference was statistically significant (P<0.05). On the seventh day following the operations, both enzymes returned to normal value in LMUDT, and OMUDT patients. In his study, other liver function indices such as TBIL, direct bilirubin (DBIL), ALP, lactic dehydrogenase (LDH), total protein (TP) and gamma glutamyltransferase (GOT) also showed derangements. TBIL and DBIL showed slight increase within 24-48 hours following operation in some patients, but the changes were within normal range, and these values returned to preoperative levels (25). These changes appear transient as the raised liver enzymes and bilirubin levels returned to their prospective values or within normal limits after a gap of 72 hours. However they may still cause worry to the surgeon regarding the integrity of the biliary tree. However our study points towards the possibility that ALP will then become important in drawing a conclusion and persistent elevation of this parameter may be suggestive of breach in integrity of biliary tree before resorting to further investigation which may prove costly and sometime invasive in nature.
Present study declared following points:
- The disturbances in LFT are not related to the age, sex in relation to laparoscopy;
- Pneumoperitoneum, which is the only variable not present in OC group. An intra-abdominal pressure of 12-14 mmHg of CO2 is higher than normal portal blood pressure of 7-10 mmHg, and is therefore capable of reducing portal blood flow and of causing alteration of the hepatic function;
- It seems that free radicals are generated at the end of laparoscopic procedure, possibly as a result of ischemia-reperfusion phenomenon induced by the inflation and deflation of the pneumoperitoneum;
- Another factor is to reduce the effect on hepatic function by causing less or no damage to the hepatic parenchyma/hepatocytes with cautery and this may help in liver enzymes to keep it normal.
Conclusions
Surgical manipulations, diathermy, patient position, arterial injury and CO2 pneumoperitoneum are the contributory factors for liver enzymes changes. These changes return to normal in 3-4 days after procedure and they have no clinical consequences in patients with normal hepatic function but they may still cause worry to the surgeon regarding the integrity of biliary tree. The low-pressure pneumoperitoneum or gasless laparoscopy by abdominal wall lifting could be a reasonable alternative.
Acknowledgements
We are thankful to Medical Record Department: Mrs Mamta Sharma.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Gurusamy KS, Samraj K, Davidson BR. Low pressure versus standard pressure pneumoperitoneum in laparoscopic cholecystectomy. Cochrane Database Syst Rev 2009;CD006930. [PubMed]
- Gupta R, Kaman L, Dahiya D, et al. Effects of varying intraperitoneal pressure on liver function tests during laparoscopic cholecystectomy. J Laparoendosc Adv Surg Tech A 2013;23:339-42. [PubMed]
- Avraamidou A, Marinis A, Asonitis S, et al. The impact of ischemic preconditioning on hemodynamic, biochemical and inflammatory alterations induced by intra-abdominal hypertension: an experimental study in a porcine model. Langenbecks Arch Surg 2012;397:1333-41. [PubMed]
- Al-Luwaizia KR, Hamad SO. Changes of liver enzymes and serum bilirubin after laparoscopic cholecystectomy. Ann Coll Med Mosul 2013;39:113-17.
- Koirala R, Shakya VC, Khania S, et al. Rise in liver enzymes after laproscopic cholecystectomy: a transient phenomenon. Nepal Med Coll J 2012;14:223-6. [PubMed]
- Saber AA, Laraja RD, Nalbandian HI, et al. Changes in liver function tests after laparoscopic cholecystectomy: not so rare, not always ominous. Am Surg 2000;66:699-702. [PubMed]
- Hagras MA. Alterations in liver function tests following laparoscopic. Pak J Surg 2013;29:245-47.
- Krupalija A, Durić A, Pandža H, et al. The effect of pneumoperitoneum on biochemical liver functions in acute cholecystitis. BH Surgery 2012;2:25-34.
- Eryılmaz HB, Memiş D, Sezer A, et al. The effects of different insufflation pressures on liver functions assessed with LiMON on patients undergoing laparoscopic cholecystectomy. ScientificWorldJournal 2012;2012:172575.
- Glantzounis GK, Tselepis AD, Tambaki AP, et al. Laparoscopic surgery-induced changes in oxidative stress markers in human plasma. Surg Endosc 2001;15:1315-9. [PubMed]
- Cekic B, Geze S, Ozkan G, et al. The effect of dexmedetomidine on oxidative stress during pneumoperitoneum. Biomed Res Int 2014;2014:760323.
- Tauro LF, Sheethal CM, Aithala PS, et al. Evaluation of Effects of Laparoscopic Surgery on Hepatic Function. J Clin Diagn Res 2008;2:1155.
- Hasukic S. CO2-Pneumoperitoneum in Laparoscopic surgery: Pathophysiological Effects and Clinical Significance. World Journal of Laparoscopic Surgery 2014;7:33-40.
- Thudichum JL. A Treatise on Gall-Stones; their Chemistry, Pathology and Treatment. London: John Churchill and sons 2006;34:1575-81.
- Unisa S, Jagannath P, Dhir V, et al. Population-based study to estimate prevalence and determine risk factors of gallbladder diseases in the rural Gangetic basin of North India. HPB (Oxford) 2011;13:117-25. [PubMed]
- Farias IE, Morais PH, Durães Lde C, et al. Effects of carbon dioxide pneumoperitoneum on hepatic and renal morphology of rats after segmental colectomy and colonic anastomosis. Acta Cir Bras 2011;26:279-84. [PubMed]
- Tan M, Xu FF, Peng JS, et al. Changes in the level of serum liver enzymes after laparoscopic surgery. World J Gastroenterol 2003;9:364-7. [PubMed]
- Omari A, Bani-Hani KE. Effect of carbon dioxide pneumoperitoneum on liver function following laparoscopic cholecystectomy. J Laparoendosc Adv Surg Tech A 2007;17:419-24. [PubMed]
- Atila K, Terzi C, Ozkardesler S, et al. What is the role of the abdominal perfusion pressure for subclinical hepatic dysfunction in laparoscopic cholecystectomy? J Laparoendosc Adv Surg Tech A 2009;19:39-44. [PubMed]
- Ahmad NZ. Routine testing of liver function before and after elective laparoscopic cholecystectomy: is it necessary? JSLS 2011;15:65-9. [PubMed]
- Marakis G, Pavlidis T, Ballas K, et al. Alterations In Liver Function Tests Following Laparoscopic Cholecystectomy. The Internet J Surg 2006;8:245-7.
- Guven HE, Oral S. Liver enzyme alterations after laparoscopic cholecystectomy. J Gastrointestin Liver Dis 2007;16:391-4. [PubMed]
- Sakorafas G, Anagnostopoulos G, Stafyla V, et al. Elevation of serum liver enzymes after laparoscopic cholecystectomy. N Z Med J 2005;118:U1317. [PubMed]
- Bhoorasingh P, McCartney T, Simpson LK. Jaundice post laparoscopic cholecystectomy. West Indian Med J 2010;59:88-91. [PubMed]
- EL-Leathy MM, Abo El-Enin MA, Abd El Aziz IM. Subclinical Hepatic Dysfunction after Laparoscopic Surgery in Pediatrics. Annals of Pediatric Surgery 2009;5:137-40.


