Tracheo-oesophageal fistula after palliative treatment of oesophageal cancer
An 86-year-old male presented with dysphagia and was diagnosed with a locally advanced adenocarcinoma of his lower oesophagus. His initial treatment was radiotherapy (20 Gy in eight fractions) aimed at palliating his dysphagia. Initially this had good effect but 6 months later his dysphagia recurred and endoscopy showed a radiation induced stricture (30-35 cm ab oral). A 105 mm × 23 mm partially covered stent was inserted endoscopically with radiological guidance and again he had good relief of dysphagia and was able to be discharged home.
He failed to attend follow up but was readmitted 4 months later with a 2-month history of a productive cough and weakness and was diagnosed with a right middle and lower lobe pneumonia. A contrast study confirmed a tracheo-oesophageal fistula (TOF) with contrast tracking from his oesophagus to the right pulmonary tree (Figure 1A, arrow showing outline of bronchial tree).
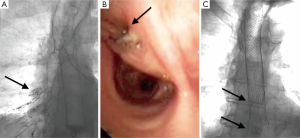
A fully covered stent (105 mm × 23 mm) was inserted endoscopically with radiological guidance to cover the fistula. Bronchoscopy prior to insertion showed the fistula to be located on the right main bronchus just after the tracheal bifurcation (Figure 1B, arrow to fistula). A contrast study 1 day after stent insertion showed good stent position and there was no contrast flow into the pulmonary tree (Figure 1C, arrows indicating distal flange of both stents).
Many patients with oesophageal cancer present with incurable disease and treatment is focussed on managing dysphagia (1,2). Options include radiotherapy, both external beam or brachytherapy, or oesophageal stenting. Radiotherapy has the advantage of providing more prolonged relief from dysphagia, however it takes several weeks for relief to be obtained and an inpatient stay may be required for enteral feeding. In contrast, oesophageal stents provide more immediate dysphagia palliation, however tumour overgrowth or obstruction can occur resulting in recurrence of symptoms (3) and they are generally recommended if life expectancy is less 3 months (4). In our institution patients are initially offered radiotherapy and if dysphagia recurs—either as a malignant recurrence or from radiation fibrosis a palliative stent is offered.
Self-expanding metallic stents (SEMS) were introduced in the nineties and have superseded rigid stents which had to be inserted via laparotomy. Tumour ingrowth into the mesh of the metal stents led to improvements in design with partially covered stents (covered with silicone or plastic) and fully covered stents developed to heal oesophageal leak or fistulae. Although self-expanding plastic stents, biodegradable stents and stents with antireflux mechanisms are also available, they have not be shown to be superior to SEMS (5).
SEMS insertion is an effective means of relieving dysphagia in a single procedure (6). Approximately 66% of patients can eat some solid foods after successful deployment. Early complications are uncommon but late complications occur in 25% of patients and include most commonly recurrent dysphagia due to stent migration or recurrent tumour overgrowth. More serious complications include stent erosion and TOF formation (2,7). It is this higher complication rate compared to radiotherapy that relegates them to second line treatment for dysphagia.
Acquired TOF can be a caused by a wide variety of pathologies, but malignancy of the oesophagus is the most common aetiology. The communication between the oesophagus and the airways results in recurrent aspirations, frequent chest infections, and poor nutrition. Subsequent mortality is common and if left untreated life expectancy is only a few weeks. TOF can occur in 2% of patients after SEMS insertion, although this figure is from a country where radiotherapy was unavailable (6). Like in our case, the typical location of these fistulae is at the proximal flange of the SEMS. Given the location of the TOF the aetiology is likely to be pressure necrosis from the stent onto radiation affected oesophagus rather than due to direct tumour extension. Prior radiotherapy does increases the risk of complications, including TOF, after SEMS insertion (8).
TOF in the context of oesophageal cancer are inoperable and first line palliative treatment is endoscopic covered stent insertion. Covered stents can be placed into the oesophagus, the trachea or bronchus or rarely into both lumens (9). The success rate of fistula closure with covered SEMS insertion is 87% to 91% (10). Once successful closure is achieved contamination of the bronchial tree stops and quality of life improves mainly due to oral nutrition recommencing (10). In our case we deployed a covered stent within the existing stent to treat the acquired TOF. Stents are often removable although in practice the ingrowth of tumour and/or hypergranulation tissue at the flanges precludes this from being able to be done safely. Leaving the partially covered stent in situ and deploying the covered stent within and proximal to it allowed us to treat the TOF in a safe and effective manner in this frail 86-year-old man.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Diamantis G, Scarpa M, Bocus P, et al. Quality of life in patients with esophageal stenting for the palliation of malignant dysphagia. World J Gastroenterol 2011;17:144-50. [PubMed]
- Martinez JC, Puc MM, Quiros RM. Esophageal stenting in the setting of malignancy. ISRN Gastroenterol 2011;2011:719575.
- Hanna WC, Sudarshan M, Roberge D, et al. What is the optimal management of dysphagia in metastatic esophageal cancer? Curr Oncol 2012;19:e60-6. [PubMed]
- Gray RT, O’Donnell ME, Scott RD, et al. Self-expanding metal stent insertion for inoperable esophageal carcinoma in Belfast: an audit of outcomes and literature review. Dis Esophagus 2011;24:569-74. [PubMed]
- Schembre D. Advances in esophageal stenting: the evolution of fully covered stents for malignant and benign disease. Adv Ther 2010;27:413-25. [PubMed]
- White RE, Parker RK, Fitzwater JW, et al. Stents as sole therapy for oesophageal cancer: a prospective analysis of outcomes after placement. Lancet Oncol 2009;10:240-6. [PubMed]
- Johnson E, Enden T, Noreng HJ, et al. Survival and complications after insertion of self-expandable metal stents for malignant oesophageal stenosis. Scand J Gastroenterol 2006;41:252-6. [PubMed]
- Kinsman KJ, DeGregorio BT, Katon RM, et al. Prior radiation and chemotherapy increase the risk of life-threatening complications after insertion of metallic stents for esophagogastric malignancy. Gastrointest Endosc 1996;43:196-203. [PubMed]
- van den Bongard HJ, Boot H, Baas P, et al. The role of parallel stent insertion in patients with esophagorespiratory fistulas. Gastrointest Endosc 2002;55:110-5. [PubMed]
- Herth FJ, Peter S, Baty F, et al. Combined airway and oesophageal stenting in malignant airway-oesophageal fistulas: a prospective study. Eur Respir J 2010;36:1370-4. [PubMed]


