Novel adjuvant therapies for pancreatic adenocarcinoma
Introduction
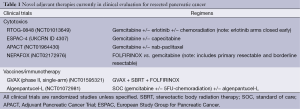
Pancreatic cancer is a very difficult-to-treat disease that the mortality rate almost mirrors the incidence worldwide (1). The majority of the patients are incurable at initial presentation with metastatic or surgically non-resectable disease (2). Only a small proportion of patients (10% to 20%) were deemed resectable at presentation but almost 80% recur within 2 years of surgical resection. The 5-year survival rate for resected patients remains approximately 20% despite adjuvant/post-operative therapy. Furthermore, a molecular analysis showed that the cancer is molecularly highly heterogeneous and each tumor harbors multiple genetic abnormalities (3). Here, we will review the current standards in adjuvant therapy briefly and novel approaches that are currently under clinical evaluation (Table 1). Neoadjuvant, or pre-operative, treatment has increasingly being adopted to improve surgical and survival outcome in ‘borderline resectable’ pancreatic cancer. However, the benefit and optimal approach to administering neoadjuvant therapy in this patient population has yet to be evaluated in randomized studies and this topic is beyond the scope of this article.
Full table
Adjuvant therapy in pancreatic cancer
The survival benefit of adjuvant treatment following surgical resection in pancreatic cancer patients had been demonstrated in randomized trials. The Gastrointestinal Tumor Study Group (GITSG) showed that fluorouracil (5FU) treatment was superior to observation only after curative resection for pancreatic cancer in improving the median overall survival (OS) (20 vs. 11 months) (4). Later, the EORTC gastrointestinal tract cancer cooperative group showed that adjuvant chemoradiation was superior to surgery alone in prolonging survival (24.5 vs. 19 months; P=0.208) (5).
The CONKO-001 trial was the first adjuvant trial to compare systemic gemcitabine treatment with observation after pancreaticoduodenectomy, and showed the superiority of gemcitabine treatment in improving median disease free survival (DFS) (13.4 vs. 6.9 months; P=0.001) and median OS (22.1 vs. 20.2 months; P=0.06) (6). The DFS improvement persisted and the OS benefit became significant in long term follow-up [hazard ratio (HR) 0.76 (95% CI, 0.61-0.95); P=0.01] (7). The role of chemotherapy and radiation was examined in the European Study Group for Pancreatic Cancer-1 (ESPAC-1) trial, using a ‘2 by 2’ factorial design evaluating observation, chemoradiotherapy alone, chemotherapy alone and chemotherapy plus chemoradiotherapy following curative resection of pancreatic cancer (8). There were a number of criticisms to the study including the lack of statistical power in the design to compare the four arms, and the non-standardized method of delivering radiation among the study sites. The results from the ESPAC-1 trial showed that patients who received chemotherapy achieved better median OS and 5-year OS than those who did not (20.1 vs. 15.5 months; 21% vs. 8%, respectively). The group who received chemoradiotherapy as part of their treatment course did not achieve survival benefit compared to those who did not receive chemoradiotherapy. The Japanese Study Group of Adjuvant Therapy for Pancreatic Cancer conducted a randomized trial that demonstrated the superiority of gemcitabine following surgery versus surgery alone in prolonging DFS (11.4 vs. 5.0 months; HR 0.60, P=0.01) though the OS did not differ significantly (22.3 vs. 18.4 months) (9). The result from the on-going RTOG-0848 trial (see below) should hopefully provide further guidance on the role of chemoradiotherapy in the adjuvant setting.
Gemcitabine and fluoropyrimidines (e.g., 5FU, capecitabine) have been the standard agents to be used in the adjuvant treatment of pancreatic cancer (10). The superiority and tolerance of these agents were evaluated in several trials. The ESPAC-3 trial showed no significant difference in survival between 5FU/folinic acid (by bolus infusion) and gemcitabine (median OS 23 vs. 23.6 months; HR 0.94, P=0.39) though gemcitabine had a more favorable toxicity profile (11). Interestingly, the JASPAC-01 trial showed that adjuvant S-1 (oral formulation of 5FU) was superior to gemcitabine in prolonging 2-year OS (70% vs. 53%) and relapse free survival (49% vs. 29%) (12). The continuous infusion mode of 5FU has long been established to be superior to the bolus infusion, and oral formulations of fluoropyrimidines (such as capecitabine, S-1) achieved pharmacokinetic profile and efficacy comparable to the continuous infusion of 5FU. Therefore, the difference in outcomes between ESPAC-3 and JASPAC-01 may be more from the pharmacokinetic characteristics related to the mode of administration than the intrinsic activity of 5FU.
The RTOG-9407 trial compared systemic 5FU versus systemic gemcitabine with interspersing 5FU-based chemoradiation. The 5FU was administered as continuous infusion for 7 days on a 4-week-on/2-week-off schedule. This study demonstrated better, but non-significant, survival outcome for gemcitabine (median OS: 20.5 vs. 17.1 months; 5-year OS: 22% vs. 18%) (13). More intensive cytotoxic regimens such as those incorporating cisplatin and epirubicin with gemcitabine and 5FU (PEFG) failed to achieve better survival and the combination therapy were more toxic than the standard agents alone (14,15).
Novel adjuvant treatments in clinical evaluation
Historically, the development of adjuvant therapy in pancreas cancer focused on evaluating drug treatments found efficacious in advanced or metastatic setting. The availability of treatment modalities with ‘less’ toxicities (e.g., vaccines) or that target novel biological processes (e.g., stem cells) offers compelling rationales to initiate their clinical development in adjuvant setting instead of advanced/metastatic patient population. However, the risk of this approach can be significant given more resource is required for adjuvant trials than those for metastatic disease.
Gemcitabine-based regimens
When combined with gemcitabine, erlotinib, a small molecule inhibitor of epidermal growth factor, achieved a marginal 2 weeks improvement in median OS in unresectable, locally advanced or metastatic pancreatic cancer patients compared to gemcitabine alone (16). The efficacy of erlotinib as adjuvant therapy in resected pancreatic cancer was evaluated in the RTOG-0848 trial (17). The RTOG-0848 trial is a randomized study that aimed to evaluate whether erlotinib and/or radiation will improve survival in resected pancreatic cancer patients. Eligible patients are randomized (Randomization #1) to either gemcitabine alone ×5 cycles (Arm 1) or gemcitabine plus erlotinib ×5 cycles (Arm 2). Upon completion, those who did not recur will be randomized (Randomization #2) to receive one additional cycle of chemotherapy assigned from Randomization #1 (Arm 3) or one cycle of chemotherapy followed by concurrent radiation with a fluorupyrimidine (Arm 4). The analysis will be stratified according to nodal status, CA19-9 level and surgical margins (R1, R0). The study was amended following the results of LAP-07 showing no survival benefit of erlotinib plus gemcitabine compared to gemcitabine alone (HR 1.19, 95% CI, 0.97-1.45; P=0.093) in locally advanced pancreatic cancer patients (18). Furthermore, the erlotinib plus gemcitabine group experienced more grade 3 and 4 adverse events than gemcitabine alone. The RTOG-0848 trial was amended to close enrollment to the erlotinib plus gemcitabine arm (Arm 2) in early-2014. The study is currently on-going to determine whether the use of concurrent fluoropyrimidine and radiotherapy will improve survival in resected pancreatic cancer patients.
Fluoropyrimidines is another anti-cancer drug class that had shown signals of efficacy in pancreatic cancer in adjuvant (as discussed above), locally advanced and metastatic settings. Capecitabine is an oral fluoropyrimidine that exerts similar pharmacokinetic and pharmacologic profile as continuous intravenous infusion of 5FU—lower peak 5FU concentration and extended exposure (19). In a phase III trial of advanced pancreatic cancer patients, capecitabine plus gemcitabine treatment achieved improvement in progression-free survival (HR 0.78; P=0.034) though the OS benefit was not statistically significant (HR 0.86; P=0.08). The meta-analysis of two additional studies evaluating the same combination (total 935 patients) showed a significant OS benefit (HR 0.86; P=0.02). The ESPAC-4 trial is a phase III multicenter randomized trial that plans to enroll 656 resected pancreatic adenocarcinoma patients to receive capecitabine plus gemcitabine or gemcitabine alone for 24 weeks (20). Enrolled patients will start treatment within 12 weeks of undergoing curative-intent surgery. The primary objective is to evaluate whether the combination arm will improve survival compared to gemcitabine alone arm, and the secondary objectives include the impact of toxicity on quality of life.
Nab-paclitaxel, or albumin bound paclitaxel, is pharmacologically superior to the Cremophor formulation with significantly less infusion hypersensitivity reactions and neutropenia (21). In the phase III MPACT trial, the addition of nab-paclitaxel to gemcitabine significantly improved median OS of metastatic pancreatic cancer patients from 6.7 to 8.5 months (HR 0.72; P<0.001) (22). The response rate was three folds higher in the nab-paclitaxel plus gemcitabine arm than gemcitabine alone. The role of nab-paclitaxel in adjuvant setting is now being evaluated in the phase III Adjuvant Pancreatic Cancer Trial (APACT) that plans to randomize approximately 800 patients following surgical resection to receive nab-paclitaxel plus gemcitabine or gemcitabine alone for six cycles (23). The analysis will be stratified according to resection status (R0, R1), nodal status and region. Patients who received prior neoadjuvant and radiation treatment are excluded, and the primary endpoint of the study is DFS. The clinical trial also includes quality-of-life evaluation.
FOLFIRINOX
The success of an intensive cytotoxic combination consisting of 5FU, leucovorin, irinotecan and oxaliplatin (FOLFIRINOX) was a major milestone in the field. The PRODIGE 4/ACCORD 11 trial is a randomized phase II/III trial that enrolled 342 patients with metastatic pancreatic cancer to receive FOLFIRINOX or gemcitabine alone (24). The combination regimen significantly improved the median OS from 6.8 to 11.1 months (HR 0.57; P<0.001). Toxicities from FOLFIRINOX treatment were significant and included febrile neutropenia, fatigues, diarrhea and peripheral neuropathy. Plan is underway to evaluate FOLFIRINOX in resectable pancreatic cancer patients. The NEPAFOX is a randomized multi-center phase II/III study that plans to enroll patients with primary resectable or borderline resectable pancreatic ductal adenocarcinoma (ClinicalTrials.gov# NCT02172976). Eligible patients will be randomized to receive surgery followed by six cycles of gemcitabine adjuvant treatment (24 weeks) or six cycles FOLFIRINOX neoadjuvant treatment (12 weeks), surgery followed by six cycles FOLFIRINOX adjuvant treatment (12 weeks). The primary endpoint is OS assessed up to 24 months, and secondary endpoints include progression-free survival, perioperative morbidity and mortality and R0 resection rate. The feasibility and tolerability of FOLFIRINOX in this localized resectable patient population will also be evaluated.
Immunotherapy and vaccines
Immunotherapy has long been a focus of anti-cancer therapy development. Immune checkpoint modulators, e.g., anti-CTLA4, anti-PD1/PD-L1, has been successful in improving survival in cancer types such as melanoma, renal cell carcinoma and lung but their role in pancreatic cancer remains unclear. Evidence suggest that the microenvironment of pancreatic adenocarcinoma is characteristically immunosuppressive, and the successful immunotherapy in the disease is likely to be more complicated (25). Vaccine therapy focus on sensitizing the host’s immune cells to antigens that are preferentially expressed in the pancreas cancer cells and not by non-cancerous ‘normal’ cells (26). Currently, there are two cancer vaccines in late-stage clinical evaluation that are modified to enhance the uptake of cancer antigens by the antigen-presenting cells (APCs).
GVAX is an allogenic vaccine developed from irradiated human pancreatic cancer cell lines (Panc10.05, Panc6.03) that have been transfected with human GM-CSF gene to secrete high level of GM-CSF at the injection site (27). The increased GM-CSF level attracts and enhances the activity of APCs that then migrate to lymphoid tissues to activate CD4+ and CD8+ cells. The vaccine was evaluated in a phase II clinical trial of 60 pancreatic cancer patients following curative-intent surgical resection (28). Enrolled patients received the first intradermal vaccine 8 to 10 weeks after surgical resection, and subsequently received adjuvant 5FU chemotherapy and chemoradiation per the RTOG-9704 standard arm. Upon the completion of adjuvant treatment, up to three additional vaccine treatments were given at 1 month interval and a final (5th dose) boost was administered 6 months after the 4th vaccine dose. The median and 1-year DFS were 17.3 months and 67.4% respectively, and the median and 1-year OS were 24.8 months and 85% respectively; compared to median OS 17.1 months in the RTOG-9704 standard arm (13). Given the encouraging result, the vaccine is being evaluated in combination with FOLFIRINOX and radiation as adjuvant therapy in resected pancreatic cancer patients (ClinicalTrials.gov# NCT01595321).
Algenpantucel-L vaccine consists of irradiated human pancreatic cancer cell lines (HAPa-1 and HAPa-2) genetically modified to express α-Gal through retroviral insertion of murine GGTA1 gene (29). The α-Gal glycoprotein is evolutionarily absent on human cells; instead, human has high level of anti-Gal antibody in the circulating immunoglobulins (30). The binding of anti-Gal antibody to α-Gal epitope thus induces hyperacute graft rejection cascade in human bodies by activating complement-mediated lysis and antibody-dependent cell-mediated cytotoxicity that destroy the α-Gal-expressing cells. The intradermal injection of algenpantucel-L therefore harness such hyperacute rejection process to enhance the tumor-related antigen uptake by the APCs that then migrate to regional lymph nodes to activate the CD4+ and CD8+ cells. The vaccine was evaluated in adjuvant setting in a phase II multi-institutional study enrolling pancreatic cancer patients following R0 or R1 surgical resection (29). Enrolled patients received adjuvant treatment using gemcitabine and 5FU-based chemoradiotherapy per the RTOG-9704 trial, and received either 100 or 300 million cells per dose. The vaccination starts within 6 weeks after surgery without chemotherapy on days 1 and 8 (Cycle 1). Cycle 2 starts 1 week after the second vaccination when patients received gemcitabine 1,000 mg/m2 weekly ×3 followed by 1 week off, concurrently with vaccination on days 1 and 15. Vaccinations then occur on days 1, 15, 29 and 43 during subsequent 5FU-based chemoradiation. Thereafter, patients receive gemcitabine and algenpantucel-L vaccine as per Cycle 1 for another three cycles. The median and 1-year DFS were 21 months and 62% respectively; 1-year OS was 86%. Given the encouraging result, algenpantucel-L vaccine is being evaluated in two phase III trials: as adjuvant therapy in resected patients (ClinicalTrials.gov# NCT01072981), and borderline resectable and locally advanced patients (ClinicalTrials.gov# NCT01836432).
Conclusions
Surgical resection remains the only curative therapy for pancreatic cancer and the median survival remains approximately 20 months despite contemporary adjuvant treatments with chemotherapy and chemoradiotherapy. Recent advances in metastatic setting using highly active chemotherapy combination regimens such as FOLFIRNOX and gemcitabine/nab-paclitaxel has led to the launch of several phase III adjuvant trials for resected pancreatic cancer patients. The impact of these combination cytotoxic regimens on the quality-of-life in this ‘disease-free’ patient population will be as important as the efficacy. Cancer vaccines evaluated so far have favorable toxicity profile and early trials suggest promising potential as adjunct to standard adjuvant treatment in resected pancreatic cancer patients. The success of this modality in phase III trial is potentially groundbreaking. In summary, a number of novel treatments consisting of cytotoxics and vaccine/immunotherapy are currently been evaluated in pancreatic cancer patients as adjuvant therapy following curative resection. Given the molecular and genetic heterogeneity of the disease, it is equally important for the integration of prognostic and predictive biomarker studies in these large randomized trials.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Hariharan D, Saied A, Kocher HM. Analysis of mortality rates for pancreatic cancer across the world. HPB (Oxford) 2008;10:58-62. [PubMed]
- Hidalgo M. Pancreatic cancer. N Engl J Med 2010;362:1605-17. [PubMed]
- Jones S, Zhang X, Parsons DW, et al. Core signaling pathways in human pancreatic cancers revealed by global genomic analyses. Science 2008;321:1801-6. [PubMed]
- Kalser MH, Ellenberg SS. Pancreatic cancer. Adjuvant combined radiation and chemotherapy following curative resection. Arch Surg 1985;120:899-903. [PubMed]
- Klinkenbijl JH, Jeekel J, Sahmoud T, et al. Adjuvant radiotherapy and 5-fluorouracil after curative resection of cancer of the pancreas and periampullary region: phase III trial of the EORTC gastrointestinal tract cancer cooperative group. Ann Surg 1999;230:776-82; discussion 782-4. [PubMed]
- Oettle H, Post S, Neuhaus P, et al. Adjuvant chemotherapy with gemcitabine vs observation in patients undergoing curative-intent resection of pancreatic cancer: a randomized controlled trial. JAMA 2007;297:267-77. [PubMed]
- Oettle H, Neuhaus P, Hochhaus A, et al. Adjuvant chemotherapy with gemcitabine and long-term outcomes among patients with resected pancreatic cancer: the CONKO-001 randomized trial. JAMA 2013;310:1473-81. [PubMed]
- Neoptolemos JP, Stocken DD, Friess H, et al. A randomized trial of chemoradiotherapy and chemotherapy after resection of pancreatic cancer. N Engl J Med 2004;350:1200-10. [PubMed]
- Ueno H, Kosuge T, Matsuyama Y, et al. A randomised phase III trial comparing gemcitabine with surgery-only in patients with resected pancreatic cancer: Japanese Study Group of Adjuvant Therapy for Pancreatic Cancer. Br J Cancer 2009;101:908-15. [PubMed]
- Tempero MA, Malafa MP, Behrman SW, et al. Pancreatic adenocarcinoma, version 2.2014: featured updates to the NCCN guidelines. J Natl Compr Canc Netw 2014;12:1083-93. [PubMed]
- Neoptolemos JP, Stocken DD, Bassi C, et al. Adjuvant chemotherapy with fluorouracil plus folinic acid vs gemcitabine following pancreatic cancer resection: a randomized controlled trial. JAMA 2010;304:1073-81. [PubMed]
- Sudo K, Nakamura K, Yamaguchi T. S-1 in the treatment of pancreatic cancer. World J Gastroenterol 2014;20:15110-8. [PubMed]
- Regine WF, Winter KA, Abrams R, et al. Fluorouracil-based chemoradiation with either gemcitabine or fluorouracil chemotherapy after resection of pancreatic adenocarcinoma: 5-year analysis of the U.S. Intergroup/RTOG 9704 phase III trial. Ann Surg Oncol 2011;18:1319-26. [PubMed]
- Schmidt J, Abel U, Debus J, et al. Open-label, multicenter, randomized phase III trial of adjuvant chemoradiation plus interferon Alfa-2b versus fluorouracil and folinic acid for patients with resected pancreatic adenocarcinoma. J Clin Oncol 2012;30:4077-83. [PubMed]
- Reni M, Balzano G, Aprile G, et al. Adjuvant PEFG (cisplatin, epirubicin, 5-fluorouracil, gemcitabine) or gemcitabine followed by chemoradiation in pancreatic cancer: a randomized phase II trial. Ann Surg Oncol 2012;19:2256-63. [PubMed]
- Moore MJ, Goldstein D, Hamm J, et al. Erlotinib plus gemcitabine compared with gemcitabine alone in patients with advanced pancreatic cancer: a phase III trial of the National Cancer Institute of Canada Clinical Trials Group. J Clin Oncol 2007;25:1960-6. [PubMed]
- Abrams RA. RTOG 0848 Protocol Information Minimize. Available online: http://www.rtog.org/ClinicalTrials/ProtocolTable/StudyDetails.aspx?study=0848
- Hammel P, Huguet F, Van Laethem JL, et al. Comparison of chemoradiotherapy (CRT) and chemotherapy (CT) in patients with a locally advanced pancreatic cancer (LAPC) controlled after 4 months of gemcitabine with or without erlotinib: Final results of the international phase III LAP 07 study. J Clin Oncol 2013;31:LBA4003a.
- Cunningham D, Chau I, Stocken DD, et al. Phase III randomized comparison of gemcitabine versus gemcitabine plus capecitabine in patients with advanced pancreatic cancer. J Clin Oncol 2009;27:5513-8. [PubMed]
- Neoptolemos J. ESPAC-4: EUROPEAN STUDY GROUP FOR PANCREATIC CANCER - TRIAL 4. Combination versus single agent chemotherapy in resectable pancreatic ductal and peri-ampullary cancers. Available online: http://public.ukcrn.org.uk/search/StudyDetail.aspx?StudyID=4307
- Ma WW, Hidalgo M. The winning formulation: the development of paclitaxel in pancreatic cancer. Clin Cancer Res 2013;19:5572-9. [PubMed]
- Von Hoff DD, Ervin T, Arena FP, et al. Increased survival in pancreatic cancer with nab-paclitaxel plus gemcitabine. N Engl J Med 2013;369:1691-703. [PubMed]
- Tempero MA, Cardin DB, Biankin A, et al. APACT: A phase 3 randomized, open-label, multicenter trial evaluating the use of adjuvant nab-paclitaxel (nab-P) plus gemcitabine (G) versus G alone in patients (pts) with surgically resected ductal pancreatic adenocarcinoma (PDA). J Clin Oncol 2014;32:abstr TPS4162.
- Conroy T, Desseigne F, Ychou M, et al. FOLFIRINOX versus gemcitabine for metastatic pancreatic cancer. N Engl J Med 2011;364:1817-25. [PubMed]
- Inman KS, Francis AA, Murray NR. Complex role for the immune system in initiation and progression of pancreatic cancer. World J Gastroenterol 2014;20:11160-81. [PubMed]
- Chen DS, Mellman I. Oncology meets immunology: the cancer-immunity cycle. Immunity 2013;39:1-10. [PubMed]
- Jaffee EM, Hruban RH, Biedrzycki B, et al. Novel allogeneic granulocyte-macrophage colony-stimulating factor-secreting tumor vaccine for pancreatic cancer: a phase I trial of safety and immune activation. J Clin Oncol 2001;19:145-56. [PubMed]
- Lutz E, Yeo CJ, Lillemoe KD, et al. A lethally irradiated allogeneic granulocyte-macrophage colony stimulating factor-secreting tumor vaccine for pancreatic adenocarcinoma. A Phase II trial of safety, efficacy, and immune activation. Ann Surg 2011;253:328-35. [PubMed]
- Hardacre JM, Mulcahy M, Small W, et al. Addition of algenpantucel-L immunotherapy to standard adjuvant therapy for pancreatic cancer: a phase 2 study. J Gastrointest Surg 2013;17:94-100; discussion p. 100-1.
- Galili U. The alpha-gal epitope and the anti-Gal antibody in xenotransplantation and in cancer immunotherapy. Immunol Cell Biol 2005;83:674-86. [PubMed]


