Exfoliative erythroderma as a paraneoplastic presentation of adenocarcinoma of the gallbladder
Introduction
Gall bladder carcinoma (GBC) is a rare GI malignancy. Worldwide, there is a prominent geographic variability in GBC incidence that correlates with the prevalence of cholelithiasis. High rates of GBC are seen in South American countries as well as some areas of India, Pakistan, Japan and Korea (1,2). We are presenting a case of gall bladder adenocarcinoma presenting with a paraneoplastic syndrome in the form of exfoliative erythroderma. This is a very rare presentation of gall bladder malignancy, which by itself is an uncommon malignancy. North America is considered a low incidence area. Estimates from the surveillance, epidemiology and end results (SEER) database reveal an incidence of 1 to 2 cases per 100,000 populations in the US (3).
Case report
A 71-year-old white male presented with a skin rash which was exfoliating, crusted appearing, and spread all over the patient’s body associated with occasional itching (Figure 1) the skin rash had developed over the previous month and had progressively spread to all over the body. The only medications that the patient was taking were iron supplements for iron deficiency anemia and afzulosin for prostatic hypertrophy. Both these medications were stopped on appearance of the rash without any resolution. The patient as an outpatient also went to a dermatologist who prescribed him a course of oral prednisone without any improvement. The patient thus decided to come to the emergency room for further management. Interestingly, on further looking back the medical records it was seen that the patient had presented to the hospital 6 months ago after an episode of fall from a ladder. At that time, he had an evaluation in the emergency department where a CAT scan of chest and abdomen (Figure 2) was performed which showed a comminuted displaced fracture of the left clavicular head that was treated with a sling and also compression fracture of the L2 vertebral body that was treated conservatively with pain medications. Co-incidentally at that time a liver mass was also seen on the CT scan described as a 5.6 cm × 5.2 cm rim enhancing heterogeneous mass in the right hepatic lobe abutting the gall bladder. High attenuation with nodularity was seen in the gallbladder fundus. The common bile duct was dilated, measuring 1.4 cm. The patient was instructed to follow up for that mass at that time but was lost to follow up. The patient also noted a 25 pound weight loss in the 3 months prior to presentation. No abdominal pain or any other symptoms suggestive of the presence of intra-abdominal mass or obstructive jaundice were noted apart from the rash and itching. Patient used to drink 1-2 beers per day in most of day of weeks and the patient’s body mass index was noted to be 22.9 kg/m2. Family history was significant for colon cancer.

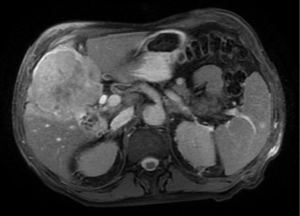
On admission the routine labs showed microcytic hypochromic anemia with hemoglobin of 8.8 gram/DL. Liver, kidney function tests were found to be normal. Alfa-fetoprotein and CEA levels were not elevated. C-reactive protein was 93.1 mg/L and ESR was 29 mm/hour. Ferritin was 590 nanogram/mL but iron saturation was 7% and iron level was 12 mcg/DL thus indication a mixed iron deficiency anemia and anemia of chronic disease. Hepatitis viral panel was found to be negative. ANA and anti-smooth muscle antibody were weakly positive. The patient then had an MRI of the abdomen (Figure 3) that showed interval enlargement of that heterogeneously enhancing large soft tissue mass originating from the gallbladder wall and into the surrounding hepatic parenchyma measuring approximately 9.1 cm × 7.7 cm in greatest dimension. This likely represented a gallbladder carcinoma, infiltrating the surrounding hepatic parenchyma. Cholelithiasis, abdominal ascites and Splenomegaly were also noted on the MRI.
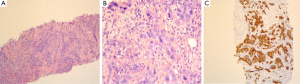
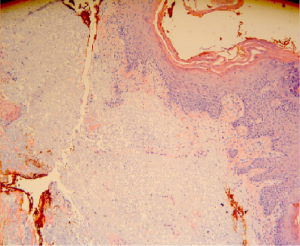
Patient had a biopsy from the gallbladder mass via a trans-hepatic route under ultrasound guidance. Biopsy showed (Figure 4) adenocarcinoma with negative stains includes CK7, CK20, and HSA (HepPAR). Skin biopsy (Figure 5) was taken from the right elbow that came back with non-specific finding in the form of benign skin with marked solar elastosis and mild perivascular lymphocytic infiltrate.
The patient was then transferred to another facility and underwent resection of the gall bladder mass. Two weeks after the removal of the mass, complete resolution of the skin rash was observed. The patient was then advised to follow up with the oncology clinic as an outpatient for further management.
Discussion
Gallbladder cancer is a rare disease that often arises in the setting of chronic inflammation. The American Cancer Society estimates that approximately 10,000 new cases of gallbladder cancer and other biliary cancers will be diagnosed in 2013 (4).
Gallbladder cancer arises in the setting of chronic inflammation. In the vast majority of patients (>75%), the source of this chronic inflammation is cholesterol gallstones. The presence of gallstones increases the risk of gallbladder cancer 4- to 5-fold (5). Other more unusual causes of chronic inflammation are also associated with gallbladder cancer. These causes include primary sclerosing cholangitis, ulcerative colitis (6), liver flukes, chronic Salmonella typhi and paratyphi infections (7), and Helicobacter infection (8). Usual clinical presentations are steady pain in the upper right abdomen, weakness, loss of appetite, weight loss, jaundice and vomiting due to obstruction.
We report a case of gall bladder adenocarcinoma with the only presenting symptom of exfoliative erythroderma all over the body associated with itching. Erythroderma was considered as a paraneoplastic syndrome secondary to the gall bladder malignancy. The only case with a similar presentation was seen in 2005 reported by Kameyama et al. in Japan (9). While Kameyama reported the case in a Japanese male, our case is reported in a Caucasian male in whom the incidence of GBC is rare as compared to the Japanese. The lowest incidence rate for gallbladder cancer is among non-Hispanic white males and is 0.7 per 100,000 person-year (10). In non-Hispanic whites and blacks, the rate of gallbladder cancer rises more slowly than among Hispanic whites and American Indian/Alaskan Natives. The rates for gallbladder cancer are higher among women than men in all age groups (10).
Skin rash can provide the first clues to a diagnosis in 1% of internal malignancies (11). Erythroderma secondary to malignancies in general has been reported. A study was performed on 135 cases with erythroderma found that about one fifth of the patients had lymphomas and mycosis fungoides (12). Exfoliative erythroderma is rare secondary to GI malignancy (13).
In the case reported by Kameyama et al. (9), the skin rash spontaneously resolved following the resection of the mass. In previous cases of other gastrointestinal malignancies like gastric cancer, similar resolution of the eruption was seen following curative gastrectomy (13,14). Recurrence of the rash was seen with the recurrence of dysplasia (13). Similar resolution of the rash was seen in our patient after surgical resection of the tumor. Thus, it indicates that resolution of the erythroderma can be seen with curative resection of the tumor and its recurrence might indicate recurrence.
Thus while uncommon, it is important to keep gastrointestinal malignancies and specifically GBCs in the list if differentials when working up a patient for unexplained dermatological findings like exfoliative erythroderma.
Acknowledgements
The authors thank to the Department of Oncology, Department of Pathology and Department of Internal Medicine at Monmouth Medical Center.
Disclosure: The authors declare no conflict of interest.
References
- Strom BL, Soloway RD, Rios-Dalenz JL, et al. Risk factors for gallbladder cancer. An international collaborative case-control study. Cancer 1995;76:1747-56. [PubMed]
- Randi G, Franceschi S, La Vecchia C. Gallbladder cancer worldwide: geographical distribution and risk factors. Int J Cancer 2006;118:1591-602. [PubMed]
- Carriaga MT, Henson DE. Liver, gallbladder, extrahepatic bile ducts, and pancreas. Cancer 1995;75:171-90. [PubMed]
- What are the key statistics about gallbladder cancer? Available online: http://www.cancer.org/cancer/gallbladdercancer/detailedguide/gallbladder-key-statistics
- Lowenfels AB, Maisonneuve P, Boyle P, et al. Epidemiology of gallbladder cancer. Hepatogastroenterology 1999;46:1529-32. [PubMed]
- Bernstein CN, Blanchard JF, Kliewer E, et al. Cancer risk in patients with inflammatory bowel disease: a population-based study. Cancer 2001;91:854-62. [PubMed]
- Randi G, Franceschi S, La Vecchia C. Gallbladder cancer worldwide: geographical distribution and risk factors. Int J Cancer 2006;118:1591-602. [PubMed]
- Matsukura N, Yokomuro S, Yamada S, et al. Association between Helicobacter bilis in bile and biliary tract malignancies: H. bilis in bile from Japanese and Thai patients with benign and malignant diseases in the biliary tract. Jpn J Cancer Res 2002;93:842-7. [PubMed]
- Kameyama H, Shirai Y, Date K, et al. Gallbladder Carcinoma Presenting as Exfoliative Dermatitis (Erythroderma). Int J Gastrointest Cancer 2005;35:153-5. [PubMed]
- Schottenfeld D, Fraumeni J. eds. Cancer Epidemiology and Prevention. 3rd. New York: Oxford University Press, 2006:787-800.
- Yuste Chaves M, Unamuno Pérez P. Cutaneous manifestations of systemic malignancies: part 2. Actas Dermosifiliogr 2013;104:543-53. [PubMed]
- Nicolis GD, Helwig EB. Exfoliative dermatitis. A clinicopathologic study of 135 cases. Arch Dermatol 1973;108:788-97. [PubMed]
- Harper TG, Latuska RF, Sperling HV. An unusual association between erythroderma and an occult gastric carcinoma. Am J Gastroenterol 1984;79:921-3. [PubMed]
- Sunami K, Taniguchi H, Moriyama T, et al. Papuloerythroderma associated with gastric cancer; report of a case. Nihon Shokakibyo Gakkai Zasshi 1995;92:1285-8. [PubMed]



