Systemic treatment of gastric and esophageal adenocarcinoma in elderly patients
Cancer of the stomach and of the gastro-esophageal junction (GEJ) are diseases of older individuals. The median age for stomach cancer worldwide is 61 (1). While the incidence of cancer of the fundus is declining in the USA, the incidence of cancer of the cardia and of the GEJ is increasing in all age groups and particularly among individuals 65 and older (2).
The treatment of cancer with chemotherapy in the older aged person involves two types of questions: Is the cancer susceptible to the treatment? Is the treatment going to be beneficial? To answer the second question it is necessary to estimate the patient’s life-expectancy and the ability to tolerate the treatment, termed functional reserve.
Is the cancer different in older individuals?
At present, there is no conclusive evidence that the biology of stomach and lower esophageal cancer changes with age. This statement is based on review of pathology, molecular markers, and genomic data. In general, younger age may be associated with more aggressive tumors, with a higher prevalence of linitis plastica and advanced stage (3).
Since 1965 adenocarcinoma of the stomach and of the GEJ has been described as intestinal type or diffuse (4). The diffuse type is an independent poor prognostic factor for survival. Since the original classification, the prevalence of the two types changed with age and the poor prognosis diffuse type became less common with increasing age (4).
It is clear that different molecular steps are involved in the pathogenesis of the two different tumors, but it is not clear which of these steps may be responsible for the difference in aggressiveness (5). Unlike other cancers, it has not been clearly established whether different genomic profiles purport different prognoses in cancer of the gastric cardia (5-7). A recent report from China described the intestinal stem cell marker LGR5, as a poor prognostic factor for stomach cancer and found that the prevalence of this marker increased after age 55 (8).
In the case of adenocarcinoma of the esophagus, a number of biomarkers, including COX2, VEGF, cyclin D and survivin, appear associated with a shorter patient survival (9). It is not clear whether the prevalence of these changes varies with age. Recently, a 3-gene panel was reported to be associated with decreased survival in adenocarcinoma of the esophagus (10), and the prevalence of these genetic changes increased with the age of the patients. Two of the many molecular markers identified in adenocarcinoma of the stomach and of the lower esophagus are targets for therapeutic interventions, HER2 and VEGF (6). It does not appear that the prevalence of these markers changes with age.
In conclusion, the evidence related to the interaction of the biology of adenocarcinoma of the stomach and lower esophagus and age is confusing and somehow contradictory. Though the prevalence of clinically aggressive gastric cancer appears to decrease with age, one cannot find any indication to change the type of systemic treatment, chemotherapy or biological therapy, according to the age of the patients.
Who are the elderly and what are the consequences of age on cancer treatment?
Aging is associated with a progressive reduction in functional reserve and with an increased prevalence of chronic diseases and of debilitating conditions referred to as geriatric syndromes (11). This association leads to increased susceptibility to diseases and to stress, resulting in an increased risk of death. The prevalence of functional disability and functional dependence also increases with age (12). Functional dependence implies that a person is not able anymore to perform by her/himself the basic activities of daily living (ADL) or the instrumental activities of daily living (IADL). This person may need the assistance of a caregiver to survive. The ADLs include continence, transferring, feeding, grooming, dressing, and toileting. The IADLs include use of transportation, ability to go shopping, to providing one’s meal, to use the telephone, and to manage one’s finances. Loss of functional dependence may have different causes that may include decreased eyesight or hearing, debilitating conditions such as a stroke, and increased prevalence of the so called geriatric syndromes such as dementia, severe depression, delirium following mild infections or medications, dizziness, falls, fractures, incontinence, neglect and abuse, and failure to thrive (13). Functionally dependent individuals may not be able to obtain adequate medical treatment in the absence of a caregiver, and for this reason the evaluation of the socio-economic context is extremely important prior to planning the treatment of cancer in an older aged person. As the need for home caregivers is increasing with the aging of the population, the pool of potential caregivers is shrinking due reduced birth rate, dissolution of the extended family, and full employment of women (14).
While aging is universal it occurs at different rates in different individuals. The chronologic age of a person does not reflect the physiologic age that is of interest in medical decisions. The assessment of the physiologic age involves the estimate of a person life expectancy and tolerance of the planned treatment (12).
A number of laboratory tests may predict life expectancy. The so called inflammatory index (15) has been validated in two large cohort studies of aging individuals: the in Chianti and the Baltimore longitudinal study. The index is obtained by adding together the log of the circulating concentration of interleukin 6 and two logs of the concentration of the tumor necrosis factor receptor 2. Aging is associated with a progressive and chronic inflammation and the concentration of inflammatory markers predicts the risk of mortality, of cardiovascular diseases, and of geriatric syndromes. The inflammatory index has not been validated yet in cancer patients. Seemingly, the presence of cancer may be responsible of increased concentration of inflammatory markers that may decline once the cancer is in remission. The length of leukocyte telomeres is inversely related to life expectancy and stress tolerance (16). In epidemiological studies, this assay may be very helpful to study the association of age with disease, disability and death. However, the wide inter-individual variation in telomere length may make it unsuitable to estimate individual physiologic age (17). Other markers of aging include the expression of the gate-keeper gene p16 NIK4a in normal tissues (18). This assay is promising but it requires biopsy sampling of normal tissues.
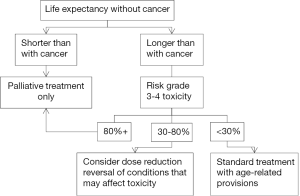
A comprehensive geriatric assessment (CGA), involving function, assessed as ADLs and IADLs, the presence of geriatric syndromes, polymorbidity, polypharmacy, emotional and cognitive disorders, and socioeconomic status (with special emphasis on the presence and the adequacy of the caregiver) is currently the best validated instrument for estimating a person’s physiologic age (19). Based on the CGA, one may estimate a person’s risk of mortality with and without cancer up to 9 years post diagnosis (20) as well as the risk of chemotherapy induced toxicity (21,22). Based on the geriatric assessment, the risks and benefits of cancer treatment in the individual patients may be estimated and the treatment may be personalized (Figure 1).
The figure represents a reasonable suggestion of how to incorporate the principles of geriatric medicine in the treatment of cancer. Of course, every final decision will have to be negotiated with the patient and his caregiver(s). For some individuals, the risk of serious toxicity of 30% may be so high as to preclude acceptance of any treatment able to prolong survival for just a few months, while for others, the same few months of life may be worthwhile to accept a risk of toxicity higher that 80%.
Senior adult oncologists strongly recommend that all patients whose disease is incurable receive a palliative care consult at the beginning of treatment. In patients with metastatic non-small cell lung cancer, this approach has resulted in improved survival and decreased cost due to the reduction in futile and possibly harmful care (23).
Reversible conditions that may increase the risk of toxicity include de-conditioning and malnutrition that are common in older individuals who have been bedridden for a prolonged period of time, acute diseases, poorly controlled chronic illnesses, polypharmacy with a high risk of drug-drug interactions (24), and an absent or inadequate caregiver.
An unsolved question concerns which patients should have a CGA. It is recommended at present that all individuals 70 and older undergo, at the very least, some form of geriatric screening to establish whether they may benefit from the full CGA (19). The age threshold of 70 was selected because it is between age 70 and 75 when the incidence of age-related changes start increasing more steeply. It should be underlined that age 70 does not define older physiologic age. It is simply a threshold beyond which the majority of physiologically old individuals are found.
A number of special precautions are indicated in all older cancer patients receiving chemotherapy (19) irrespective of the patient’s functional status. Age is associated with an almost universal drop in glomerular filtration rate and for this reason it is suggested that the first dose of a medication be adjusted according to the estimated creatinine clearance of each patient. Age is also associated with a decline in the hematopoietic reserve and for this reason it is recommended that individuals 65 and older be treated prophylactically with filgrastim or pegfilgrastim when receiving chemotherapy with a risk of myelotoxicity comparable to CHOP.
The management of cancer of the stomach and of the lower esophagus may involve a platinum derivative or a taxane. The neurological condition of these patients should be monitored at each visit as peripheral neuropathy is more common and more debilitating in older individuals and may also be irreversible. Another chemotherapy-related complication whose risk increases with age is cardiotoxicity. Anthracyclines are now seldom used for the management of these cancers, but approximately 25% of patients may be eligible to receive trastuzumab, a monoclonal antibody that may cause a generally reversible decline in ejection fraction.
Conclusions
The incidence and the prevalence of adenocarcinoma of the stomach and of the lower esophagus increase with age. The biology of these diseases may not change with age, but the benefit of chemotherapy may decline due to a reduction in life expectancy and an increased risk of treatment related complications. We recommend that the treatment of individuals 70 and over with these malignancies be personalized based on life expectancy and risk of complications. The CGA is currently the instrument best validated for assessing these parameters.
Acknowledgements
Disclosure: The author declares no conflict of interest.
References
- Pelucchi C, Lunet N, Boccia S, et al. The stomach cancer pooling (StoP) project: study design and presentation. Eur J Cancer Prev 2015;24:16-23. [PubMed]
- Brown LM, Devesa SS, Chow WH. Incidence of adenocarcinoma of the esophagus among white Americans by sex, stage, and age. J Natl Cancer Inst 2008;100:1184-7. [PubMed]
- Park JC, Lee YC, Kim JH, et al. Clinicopathological aspects and prognostic value with respect to age: an analysis of 3,362 consecutive gastric cancer patients. J Surg Oncol 2009;99:395-401. [PubMed]
- Qiu MZ, Cai MY, Zhang DS, et al. Clinicopathological characteristics and prognostic analysis of Lauren classification in gastric adenocarcinoma in China. J Transl Med 2013;11:58. [PubMed]
- Yakirevich E, Resnick MB. Pathology of gastric cancer and its precursor lesions. Gastroenterol Clin North Am 2013;42:261-84. [PubMed]
- Zali H, Rezaei-Tavirani M, Vafaee R, et al. Gastric cardia adenocarcinoma pathway analysis. Gastroenterol Hepatol Bed Bench 2013;6:S11-8. [PubMed]
- Grabsch HI, Tan P. Gastric cancer pathology and underlying molecular mechanisms. Dig Surg 2013;30:150-8. [PubMed]
- Zheng ZX, Sun Y, Bu ZD, et al. Intestinal stem cell marker LGR5 expression during gastric carcinogenesis. World J Gastroenterol 2013;19:8714-21. [PubMed]
- Chen M, Huang J, Zhu Z, et al. Systematic review and meta-analysis of tumor biomarkers in predicting prognosis in esophageal cancer. BMC Cancer 2013;13:539. [PubMed]
- Ong CA, Shapiro J, Nason KS, et al. Three-gene immunohistochemical panel adds to clinical staging algorithms to predict prognosis for patients with esophageal adenocarcinoma. J Clin Oncol 2013;31:1576-82. [PubMed]
- Theou O, Brothers TD, Peña FG, et al. Identifying common characteristics of frailty across seven scales. J Am Geriatr Soc 2014;62:901-6. [PubMed]
- Balducci L. Studying cancer treatment in the elderly patient population. Cancer Control 2014;21:215-20. [PubMed]
- Rosso AL, Eaton CB, Wallace R, et al. Geriatric syndromes and incident disability in older women: results from the women’s health initiative observational study. J Am Geriatr Soc 2013;61:371-9. [PubMed]
- Hansen L, Archbold PG, Stewart B, et al. Family caregivers making life-sustaining treatment decisions: factors associated with role strain and ease. J Gerontol Nurs 2005;31:28-35. [PubMed]
- Varadhan R, Yao W, Matteini A, et al. Simple biologically informed inflammatory index of two serum cytokines predicts 10 year all-cause mortality in older adults. J Gerontol A Biol Sci Med Sci 2014;69:165-73. [PubMed]
- Bodelon C, Savage SA, Gadalla SM. Telomeres in molecular epidemiology studies. Prog Mol Biol Transl Sci 2014;125:113-31. [PubMed]
- Falandry C, Gilson E, Rudolph KL. Are aging biomarkers clinically relevant in oncogeriatrics? Crit Rev Oncol Hematol 2013;85:257-65. [PubMed]
- Pareja-Galeano H, Sanchis-Gomar F, Lucia A. p16INK4a, NAD(+), and sestrins: new targets for combating aging-related chronic illness? J Cell Physiol 2014;229:1575-6. [PubMed]
- Hurria A, Wildes T, Blair SL, et al. Senior adult oncology, version 2.2014: clinical practice guidelines in oncology . J Natl Compr Canc Netw 2014;12:82-126. [PubMed]
- Yourman LC, Lee SJ, Schonberg MA, et al. Prognostic indices for older adults: a systematic review. JAMA 2012;307:182-92. [PubMed]
- Extermann M, Boler I, Reich RR, et al. Predicting the risk of chemotherapy toxicity in older patients: the Chemotherapy Risk Assessment Scale for High-Age Patients (CRASH) score. Cancer 2012;118:3377-86. [PubMed]
- Hurria A, Togawa K, Mohile SG, et al. Predicting chemotherapy toxicity in older adults with cancer: a prospective multicenter study. J Clin Oncol 2011;29:3457-65. [PubMed]
- Temel JS, Greer JA, Muzikansky A, et al. Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med 2010;363:733-42. [PubMed]
- Balducci L, Goetz-Parten D, Steinman MA. Polypharmacy and the management of the older cancer patient. Ann Oncol 2013;24 Suppl 7:vii36-40. [PubMed]