Giant mucinous cystic neoplasms of pancreas and liver with unusual adipose tissue component: a case report
Introduction
Mucinous cystic neoplasms (MCN) of pancreas and liver occur very rarely. Pancreatic mucinous cystic neoplasms are reported to be 10% of all pancreatic cystic lesions and 1% of pancreatic neoplasms (1). Mucinous cystadenoma of liver comprises 5% of all hepatic cystic lesions (2). Simultaneous occurrence is even rarer, after a thorough search of Pubmed in English literature we have found 4 such cases reported before this. Three reports were of intraductal papillary mucinous tumour and one of mucinous cystadenoma with ovarian like stroma. This is the first case where the tumours were mucinous cystic neoplasms without ovarian like stroma and required a Whipple’s pancreatoduodenectomy and right hepatectomy for complete excision. Another unusual point was presence of significant amount of fat in both the tumours, more so in the pancreatic tumour, to our knowledge which has not been reported before.
Case report
A 35 year-old man presented with gradual swelling of abdomen for last 10 years. This was associated with mild pain, anorexia and moderate weight loss. There was no history of alcoholism, jaundice, vomiting, obstipation or gastro intestinal bleeding.
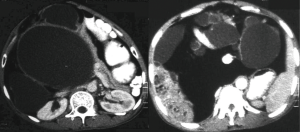
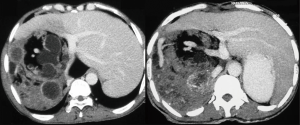
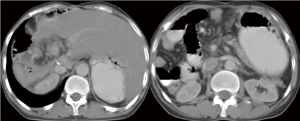
Clinical examination revealed a bosselated, abdominal swelling with soft to firm consistency occupying the whole abdomen and almost reaching up to the pelvis. His complete blood count and liver function tests were normal. An ultrasound and CECT done showed a complex hepatic mass having cystic, solid and fatty areas and a similar complex mass inside the abdominal cavity (Figures 1,2). A fine needle aspiration cytology done in another hospital was inconclusive.
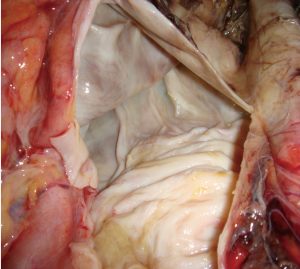
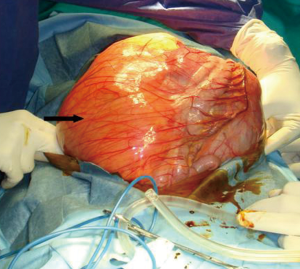
At laparotomy the peritoneal cavity was found full of a partly cystic and partly fatty mass, arising from the head of the pancreas (Figure 3). There was abundant fat around the portal triad and beneath the gallbladder. There was no ascites or peritoneal nodules. During tumour mobililization splenic vein was transected for tumor clearance. Classical Whipple’s pancreatoduodenectomy, splenectomy alongwith the tumour excision was done.
Postoperatively patient had a pancreatic leak which was managed conservatively. After 3 months, he underwent right hepatectomy for the liver tumour. At this time rest of the visceras appeared normal and no areas of abnormal adoipose tissue proliferation was seen.
Two independent experienced pathologists examined the specimens and the microscopy.
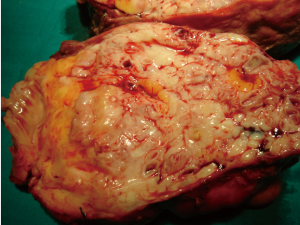
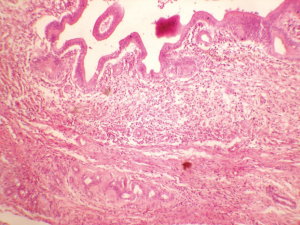
The pancreatic specimen (approximately 37 cm × 25 cm × 8 cm in size) was smooth, glistening, and grayish in color with attached clumps of fat. On cutting open it was multiloculated and cystic, largest locule was of 18 cm diameter. Inner surface was also smooth, whitish and without any papillary projections (Figure 4). Cysts contained mucoid, brown, inpissated fluid. Microscopic sections revealed mucinous neoplasm with a single layer of mucin secreting columnar epithelium. There was no cellular stratification, pleomorphism or mitotic activity (Figure 5). Sections from fat showed mature adipose tissue.
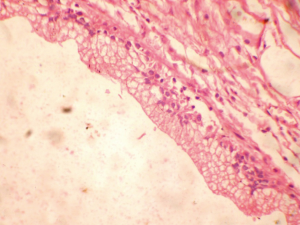
The liver specimen was of 15 cm × 9 cm × 6 cm in size, containing both solid and cystic areas of variable sizes with areas of adipose tissue (Figure 6). Largest cyst was of 3 cm diameter. Cysts contained yellowish mucoid materal. Microscopic sections showed cystic tumor with a lining of columnar mucin secreting cells having minimal cytologic atypia. Intervening fibrocollagenous stroma showed biliary ducts, scant lymphocytic and plasma cell infiltrate (Figure 7).
The final histological diagnosis was of mucinous cystic neoplasms of the pancreas and the liver without ovarian-like stroma. The patient is doing well 24 months postoperatively. Followup CECT scan done after 24 months showed no recurrence of the tumours (Figure 8).
Discussion
Simultaneous occurrence of pancreatic and hepatic MCNs is very rarely reported. After extensive search of Pubmed in English language, we have found four such reports and one report from a non-indexed (Non Pubmed) journal (Table 1). Pancreatic MCN is found in about 10% of all cystic pancreatic lesions and 1% of neoplasms. Most of the cases occur in elderly women (>95%) (1). They can present with pain abdomen, mass lesion or anorexia or can be discovered incidentally. 90% of them occur in the body or tail of the pancreas (1). Histologically the tumour is lined by tall, columnar cells containing mucin. Ovarian-like stroma is considered essential for the diagnosis of mucinous cystadenoma, whereas papillary like projections and development in the pancreatic duct is essential for the diagnosis of intraductal papillary mucinous neoplasms (2). In our case the tumour lacked ovarian like stroma, there was no papillary projections and it was not growing within the pancreatic duct. As some pathologists consider ovarian like stroma a sina qua non for diagnosis of mucinous cystadenoma, we termed the tumour in this report as “mucinous cystic neoplasm”. There was unusual amounts of fat, clump like, around the tumour and also around the portal triad and beneath the gall bladder. Fat is present in tumours like lipoma or teratoma, but we could not explain the fat deposition, peritumoural and distant to the tumour. This fat was well encapsulated and we removed the peritumoral quantity intact with the tumour, but we removed the fat piece meal around the portal traid. The gallbladder along with the fatty clumps were removed during hepatectomy. We were apprehensive about leaving behind small macroscopic amount of fat around the portal triad and its effect on recurrence of the tumour. We have followed up for 24 months and the patient is tumour free till now.
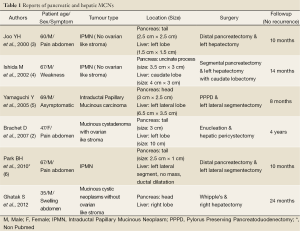
Full table
Hepatic MCN is found in about 5% of cystic hepatic lesions (2). It is common in women like its pancreatic counterpart, commonly symptomatic and single. Both the pathologists concurred that the tumors in the pancreas and the liver were histologycally similar and were in favour of the diagnosis of simultaneous occurrence of mucinous cystic neoplasm in two organs.
One of the proposed pathogenesis is these tumours are derived from the detached cells covering the gonads which is in close proximity of the liver and pancreas in the fetal period (2). But this fails to explain the presence of these tumours in men and in tumours where there is no ovarian-like stroma.
Conclusions
Liver and pancreatic mucinous cystic neoplasm occurring together is extremely rare. The presence of these tumors in a male patient puts the current hypothesis of pathogenesis in doubt. The unusual amount of fat occurred probably as a response to the tumour and it is not involved with the recurrence of the tumour as appears from the followup of the discussed patient.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Buetow PC, Rao P, Thompson LD. From the Archives of the AFIP. Mucinous cystic neoplasms of the pancreas: radiologic-pathologic correlation. Radiographics 1998;18:433-49. [PubMed]
- Brachet D, Mucci S, Desolneux G, et al. The simultaneous occurrence of mucinous cystadenomas in liver and pancreas. Eur J Gastroenterol Hepatol 2007;19:801-4. [PubMed]
- Joo YH, Kim MH, Lee SK, et al. A case of mucin-hypersecreting intrahepatic bile duct tumor associated with pancreatic intraductal papillary mucinous tumor. Gastrointest Endosc 2000;52:409-12. [PubMed]
- Ishida M, Seki K, Honda K, et al. Intraductal mucinous tumors occurring simultaneously in the liver and pancreas. J Gastroenterol 2002;37:1073-8. [PubMed]
- Yamaguchi Y, Abe N, Imase K, et al. A case of mucin hypersecreting intraductal papillary carcinomas occurring simultaneously in liver and pancreas. Gastrointest Endosc 2005;61:330-4. [PubMed]
- Park BH, Suh JH, Cha HJ, et al. Intraductal papillary mucinous tumor simultaneously involvingt the liver and pancreas-A case report. The Korean journal of pathology 2010;44: 83-6.