Common hepatic duct stricture: are lithiasis and negative brush cytology enough to rule out Klatskin tumor?
In this case report, the experience of treating a patient with clinical suspicion of hilar cholangiocarcinoma is shared and key points in differentiating from coexistent lithiasis are discussed.
Case report
An 89-year-old female presented with a 3-month history of painless jaundice and subjective weight loss. The patient had a past medical history of hypertension, aortic stenosis, hypothyroidism and hyperlipidemia. Physical examination disclosed icteric sclera and skin but no presence of right upper quadrant tenderness or mass on deep palpation. Laboratory tests were significant for profound elevation of total and direct bilirubin (23.5 and 18.9 mg/dL respectively), ALP (637 IU/L) and GGT (1,113 IU/L). Transaminases were also elevated (ALT: 323 IU/L, AST: 219 IU/L). Amylase, lipase and CBC were within normal limits.
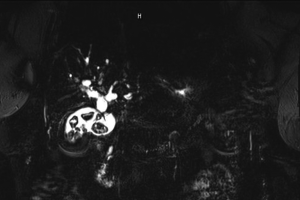
A computed tomography (CT) scan and an ultrasonogram of the abdomen showed severe dilatation of intra- and extra-hepatic biliary ducts and common bile duct as well as several gallstones without gallbladder wall thickening or pericholecystic fluid collections. MRCP further revealed choledocholithiasis and a 2 cm in length stricture in the junction of the right and left hepatic ducts, most superior portion of the common hepatic duct in the porta hepatis and upper common bile duct, highly suspicious for malignant stricture secondary to cholangiocarcinoma/Klatskin tumor (Figure 1).
ERCP with sphincterotomy and stent placement was performed, after which the patient’s obstructive jaundice improved, with bilirubin, ALP, GGT and transaminase levels trending down. Among tumor markers, carcinoembryonic antigen (CEA) was within normal limits, whereas CA 19-9 was found elevated (100 IU/L). Endoscopic brush cytology from the area of stricture was negative for presence of malignant cells. The patient refused further interventions and was discharged uneventfully after resuming diet, with continued close follow-up.
Discussion
Extra-hepatic is the most common location for biliary strictures, which may result in biochemical with or without clinical signs of obstruction. Depending on the etiology, they can be benign or malignant. Benign biliary strictures may develop from hepatolithiasis, chronic cholangitis (bacterial, parasitic, eosinophilic) as well as iatrogenic damage and ischemia. Among malignant causes, cholangiocarcinoma accounts for half of the cases, with hepatocellular carcinoma and metastatic disease occurring more rarely (1).
Intriguingly, differential diagnosis between these two large entities with entirely different management remains difficult. CA 19-9 levels have not been found able to reliably distinguish between benign and malignant causes, given that very high CA 19-9 levels may be caused by obstruction or cholangitis itself, whereas negative levels cannot rule out cholangiocarcinoma (2). Likewise, MRCP although being able to detect strictures with high sensitivity and specificity, it cannot distinguish benign from malignant strictures (3).
The need for specific tissue diagnosis has been addressed so far with several techniques including ERCP-, PTC- or EUS-mediated aspiration cytology, brush cytology or biopsy. However, submucosal tumor growth or extrinsic compression still continues to hamper proper sampling and subsequent sensitivity of the aforementioned techniques (up to 58% for brush cytology, up to 86% for biopsy) (4,5). Several efforts have been made to increase the low sensitivity of biliary cytology, including flow cytometry, digital imaging analysis, FISH, detection of K-ras and p53 mutations and CA 19-9 and CEA level measurement in bile fluid. Among them, the addition of flow cytometry to routine cytology has produced the most encouraging results (6).
Particularly, the management of patients with a stricture and concurrent choledocholithiasis is controversial, given that 10% of patients with hepatolithiasis have associated cholangiocarcinoma and reversely, up to 50% of patients with malignant biliary strictures have concurrent hepatolithiasis (1). Overall, given the need for further improvement in the accuracy of available diagnostic strategies, therapeutic decisions including observation, non-surgical treatment (endoscopic or percutaneous dilatation/stenting) and surgical resection, still depend on the clinical manifestations and the degree of clinical suspicion for malignancy.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Yeo D, Perini MV, Muralidharan V, et al. Focal intrahepatic strictures: a review of diagnosis and management. HPB (Oxford) 2012;14:425-34. [PubMed]
- Nishimura M, Naka S, Hanazawa K, et al. Cholangiocarcinoma in the distal bile duct: a probable etiologic association with choledocholithiasis. Dig Dis Sci 2005;50:2153-8. [PubMed]
- Manfredi R, Masselli G, Maresca G, et al. MR imaging and MRCP of hilar cholangiocarcinoma. Abdom Imaging 2003;28:319-25. [PubMed]
- Pugliese V, Conio M, Nicolò G, et al. Endoscopic retrograde forceps biopsy and brush cytology of biliary strictures: a prospective study. Gastrointest Endosc 1995;42:520-6. [PubMed]
- Sugiyama M, Atomi Y, Wada N, et al. Endoscopic transpapillary bile duct biopsy without sphincterotomy for diagnosing biliary strictures: a prospective comparative study with bile and brush cytology. Am J Gastroenterol 1996;91:465-7. [PubMed]
- Ryan ME, Baldauf MC. Comparison of flow cytometry for DNA content and brush cytology for detection of malignancy in pancreaticobiliary strictures. Gastrointest Endosc 1994;40:133-9. [PubMed]


